Biological Barriers
Why is it that you can't just take insulin as a tablet? The answer: Biological barriers.
Millions of diabetics have to administer this pancreatic hormone by daily injections. Insulin is one of the best selling medications throughout the world. No doubt: an insulin pill would be a major relief for most of the patients - and big business for the manufacturers.
But there is a reason why this easy and comfortable way of administration does not work: because there is a biological barrier called the intestinal epithelium. Insulin is a large molecule and cannot easily cross the intestinal wall. Moreover, since this molecule is a protein and of biological origin, insulin is degraded quickly in the bowels - which makes it a poor candidate for a medication to be swallowed. However, as soon as insulin molecules have entered the blood circulation without being degraded, they are biologically available at their target cells. Mainly in the muscles and the liver they exert their intended effect, which is to initiate the uptake of sugar.
Similar to the surface of the intestines, the skin and the tissue layers facing the airspace of the lung are also so called epithelia, and represent outer biological barriers of the human body. If one wants to administer a drug without injecting it, the first step is to get it through one of these barriers - without being degraded, if possible. In many cases, reaching the blood circulation, which is the body’s central compartment, may suffice for a drug to become biologically available.
In case a medication is aimed to work in the brain, the drug molecules must also cross the so called blood-brain barrier, which controls the transfer of substances from the circulating blood into the nervous system. In other cases, such as e.g. in cancer, infections or inflammation, the disease is localized to some specific organs or cells, and targeted drug delivery may provide additional advantages, like reducing adverse drug effects or overcoming resistance.
For drugs not only aimed to reach some extracellular receptors, but where the site of action is located inside specific cells, the membrane of the target cell may be another impediment that needs to be overcome by clever strategies. Gene therapy involves genetic material being routed to the inside of the cell, whereby "drug delivery" – the process of transporting the agent to its destination - often is the most difficult problem of the entire procedure. Drug developers address this problem, for example, by using viruses as "gene transporters". These infectious particles are basically specialised on penetrating into certain cells at high specificity and then introduce genetic material into these cells - under normal conditions, this would be their own genetic material, but in gene therapy, they carry DNA sections delivered by the biomedical experts. Alternatively, chemically produced “non-viral“ gene delivery systems are also being actively developed, especially as they promise to be safer than the viral ones.
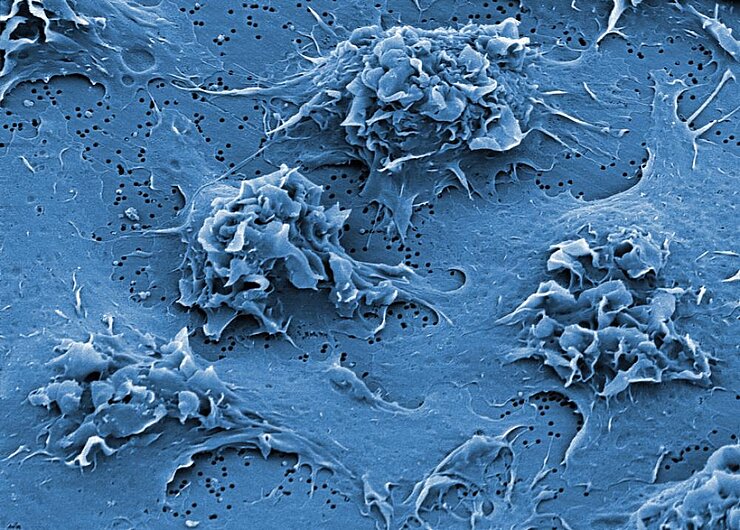
Not only the human body has biological barriers. Some antibiotics well capable of inducing the correct chemical processes in test tubes may nevertheless fail in the actual battle against infectious diseases. Biofilms produced by some bacteria to protect themselves or even cell walls surrounding each of these microorganisms may prevent the active compound from reaching its target and thus cause unexpected resistance. Besides discovering and optimizing antiinfective drug molecules, some advanced delivery technologies may thus be necessary to overcome these hurdles.
Researchers at the HZI pursue two main approaches to promote the transport of bioactive substances. They use in-vitro models based on cells and tissues to imitate the epithelia of the intestines, skin or lungs. Such an approach allows to study the properties and to directly observe transport processes occurring at a biological barrier, which would not be possible in the “black box” of an animal experiment. In addition, because these in-vitro models can be based on human cells and tissues, the translation of such experimental data to the clinical situation in human patients is facilitated.
To “package” the active substances appropriately so that they can cross the barrier more easily, HZI researchers investigate novel drug delivery systems, often based on nanotechnology (“nanomedicine”). This can, for example, be achieved by encapsulating them into a protective carrier and, if applicable, by additional coating of its shell with signalling molecules that are recognised and actively taken up by the target cells.
By the way, the in-vitro models of HZI scientists have earned acclaim outside of their field as well: since the cultured cell models imitating epithelia allow some investigations to be done which would require the use of animal experiments in conventional techniques, the developers have been granted several research awards for alternatives to animal testing.
(mbn)