Two types of rejection
“Chronic and acute rejection differ in terms of cause, progression and treatment,” says first author Dr Bastian Engel, MHH-Clinical Department of Gastroenterology, Hepatology, Infectious Diseases and Endocrinology (GHIE). “In chronic rejection, antibodies attack the blood vessels of the transplanted liver, often without noticeable liver values. Up to 50 percent of cases lead to scarring, which can cause cirrhosis of the liver and necessitate a repeat transplant.” Doctors treat the condition using traditional immunosuppressants and measures to reduce antibodies, such as plasmapheresis, and high-dose immunoglobulin administration – with varying degrees of success.
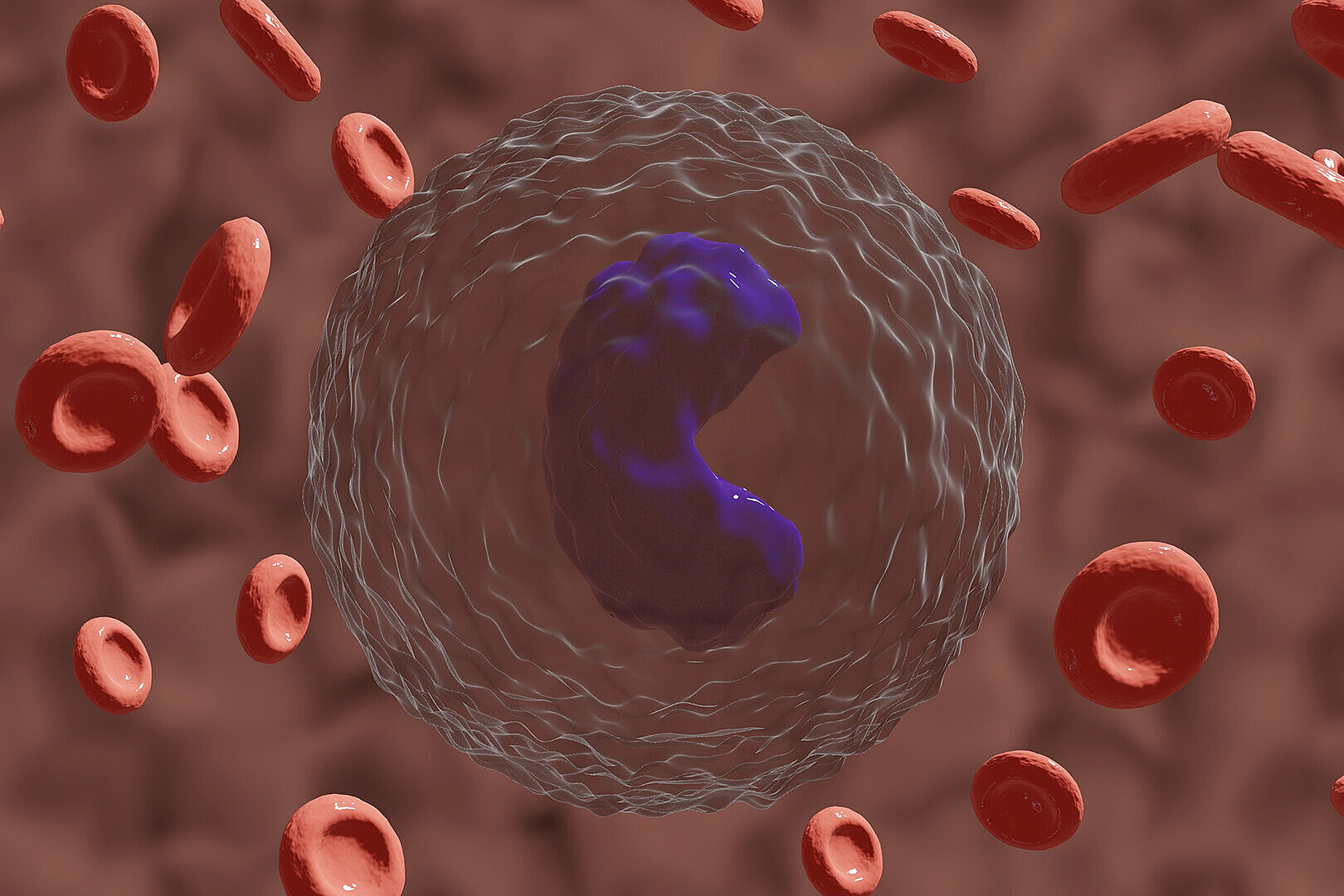
Acute rejection is easier to recognize and treat. In the process, immune cells attack the donor liver, elevating liver values and causing a deterioration in function. The risk of permanent scarring is lower, and acute rejection usually responds well to an adjustment of immunosuppression or temporary high-dose cortisone administration. “The crucial thing is that these two forms not only progress differently, but also exhibit their own molecular activity patterns – typical fingerprints in the organ. We have clearly distinguished these signatures from each other for the first time,” explains doctoral student and physician Alejandro Campos-Murguia, also a first author from the gastroenterology department.
Different treatments – a major challenge
The team analyzed for the first time which genes are active in tissue samples from liver transplant patients with and without acute and chronic rejection. The samples came from Hannover and Barcelona. “We analyzed data from gene expression, cytokines, complement factors and the extracellular matrix (ECM) – i.e. from various molecules and structures that play a role in cells and tissue – in more than 158 samples,” says Ahmed Alaswad, doctoral student at the Centre for Individualised Infection Medicine (CiiM), a joint initiative of the Helmholtz Centre for Infection Research (HZI) and the MHH, and first author. “Our analyses clearly show for the first time that signaling pathways leading to liver scarring, such as TNF–NF-κB signaling and complement activation, part of the innate immune system, indicate chronic rejection.”
Better diagnosis of rejection
The findings are more than just basic research. “The results are an important step towards personalized medicine in transplant research,” says Prof. Yang Li, co-director of the CiiM, head of the “Computational Biology for Individualised Medicine” research department at the HZI and professor at Hannover Medical School (MHH). “Our goal is for every patient to receive the best possible individualized therapy – so that they can live significantly longer with their transplanted organ.”
“In the future, these molecular signatures can help to diagnose chronic rejection in surveillance transplant biopsies earlier and more accurately, thus enabling more targeted treatment,” says Prof. Richard Taubert, senior physician at the GHIE liver transplant outpatient clinic.