HIV/AIDS
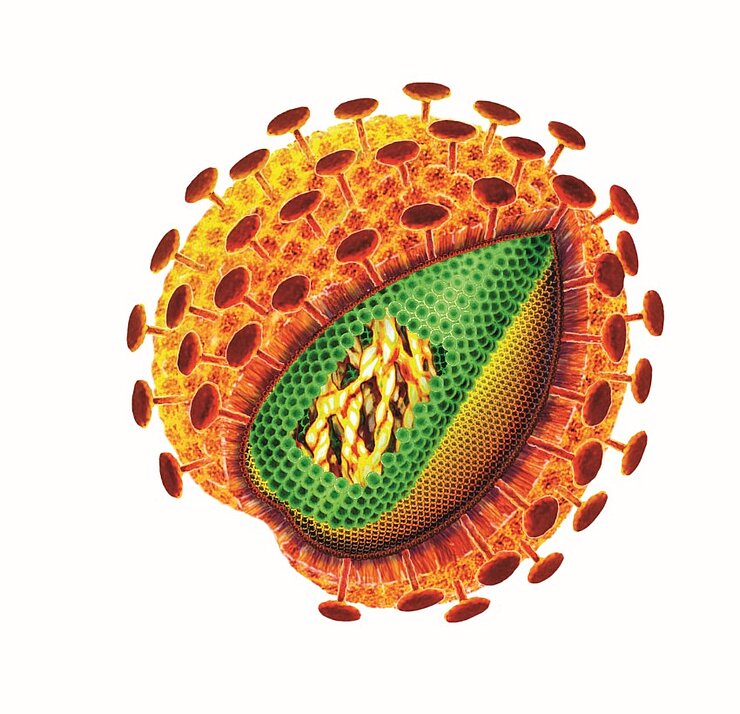
AIDS - acquired immunodeficiency syndrome - is a pandemic of global proportions and a prime example of a newly discovered pathogen's potentially devastating impact. AIDS did not begin its deadly spread until the 1980s and is thus a fairly recent addition to the current library of infectious diseases. The immunodeficiency's trigger is HIV, the human immunodeficiency virus.
The virus has decimated entire generations of people on the South African subcontinent, where it especially infects those in the 20-to-50 age range. The year 2015 witnessed some 2 million cases of new infections worldwide and 36.7 million people who were living with the virus in 2015 (source: Statista).
Another 1.1 million people died from AIDS-related causes in 2015 (source: WHO). A regional problem? Not by a longshot. The Robert Koch Institute estimates that that in Germany in 2014 approximately 84,700 people had HIV and that some 3,200 people had newly contracted the Virus.
In the end, patients do not die from HIV but from some other infection the virus helps pave the way for. HIV infects host cells with CD4 receptors on their surface. For the most part, these include certain T lymphocytes but also a number of other immune cells that are important in immune defense. HIV integrates its own genetic material into the host cell DNA, thus becoming a permanent fixture of the immune system. If the immune system now responds to some pathogen, the immune cells begin to proliferate; but instead of attacking the new intruder, they literally become HIV factories, releasing new viral particles en masse, thereby contaminating the immune system. Over the course of the incubation period, which may last up to 10 years, progressive immune cell destruction ultimately culminates in AIDS.
In Africa, the combination of HIV and tuberculosis is deadly. Those who are infected with HIV are at a 30-fold increased risk of contracting tuberculosis compared with non-HIV-patients as their immune system has been seriously weakened by the virus. In AIDS patients, tuberculosis is a normally occurring infection so that, in Africa, most HIV-related deaths can in fact be traced back to Mycobacterium tuberculosis.
In recent years, the survival rate of HIV infected persons in countries with quality health care has gone up considerably. Antiretroviral therapies (ART) are capable of reducing the viral load in the infected person's body to such an extent that the person never gets to the stage where they have full-blown AIDS. The medicines must be taken for the remainder of a person's life - and the total scope of the many adverse effects from these drugs cannot as of yet be appreciated. After all, modern-day ARTs have only been in use since the 1990s. These therapies are very costly and are only effective if patients follow a strict regimen of pill-popping - something people in countries with good health care can certainly afford to do but which is not exactly practical in Africa, the pandemic's epicenter. There are 14 million people worldwide receiving an antiretroviral therapy (source: Statista)
At this time, however, a cure is still far off. Worldwide, scientists are working on finding a vaccine in a race against time to defeat a virus that mutates extremely rapidly. This mutability makes the development of recognisable structures that could be administered in the form of a vaccine an uphill battle. At this point, an Afro-European phase IIa clinical trial for a new HIV vaccine is under way. The vaccine has to be administered by injection three times within an eight week period. If it proves successful, this could be the point where infrastructural problems start. For a comprehensive vaccination, people would need to travel to their local health center for a total of three consecutive visits to receive their scheduled shots and, in some instances, for many miles - a fact, which makes treating the disease quite difficult and which jeopardises a potential vaccine's general acceptance.
This is where scientists at the Helmholtz Centre for Infection Research come in. Their vision: to no longer inject the vaccine subcutaneously and instead administer it at the exact site where most pathogens attack: the mucous membranes. This would allow for a comprehensive vaccination of those who live farther away from a health center, increasing compliance and thus the chance of success.
(jsg)
Further Information
- Guidelines on diagnosis and therapy of HIV infection, Deutsche AIDS-Gesellschaft
- Facts on HIV/AIDS by the World Health Organization
- 2021 World AIDS Day Report of the United Nations
- Video from "TheSimpleBiology" to "HIV / AIDS"
- Website of "Deutsche Aids-Hilfe e.V." (German Aids-Aid)
- Website of "Braunschweiger Aids-Hilfe e.V." (Braunschweiger Aids-Aid)
Involved research groups
-
Genome Architecture and Evolution of RNA Viruses
 Dr Redmond Smyth
Dr Redmond Smyth -
Recoding Mechanisms in Infections
 Prof Neva Caliskan
Prof Neva Caliskan -
Vaccinology and Applied Microbiology
 Prof Dr Carlos A. Guzmán
Prof Dr Carlos A. Guzmán